Mieloma múltiple: del genoma a la medicina de precisión
Multiple myeloma: from the genome to precision medicine
Cómo citar
Descargar cita

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Mostrar biografía de los autores
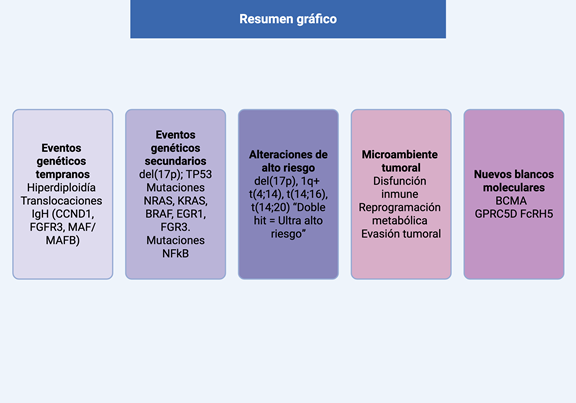
Introducción: el mieloma múltiple (MM) es un trastorno de proliferación clonal de células plasmáticas. Se caracteriza por una marcada heterogeneidad biológica y clínica. La inestabilidad genómica asociada a la maduración de las células plasmáticas origina alteraciones recurrentes, desempeñan un papel central en la patogénesis del MM. El objetivo de esta revisión es describir la arquitectura genética del MM y su impacto en el pronóstico y el tratamiento.
Métodos: se realizó una revisión de la literatura centrada en los avances recientes sobre las bases moleculares del MM, integrando hallazgos en genómica, epigenética, inmunología y microambiente tumoral con énfasis en su aplicabilidad clínica.
Resultados: las alteraciones genéticas del MM se clasifican en eventos primarios y secundarios, responsables de la iniciación y progresión de la enfermedad, asociados o no a hiperdiploidia. La interacción con el microambiente medular favorece la progresión tumoral y la evasión inmunológica. El conocimiento detallado de estas alteraciones ha permitido desarrollar escalas pronósticas que identifican a pacientes de alto riesgo candidatos a terapias más intensivas. Asimismo, se han identificado nuevos blancos terapéuticos, que han impulsado el desarrollo de terapias linfodireccionadas, incluyendo CAR-T y anticuerpos biespecíficos, con respuestas profundas y sostenidas. Un subgrupo de pacientes con citogenética favorable y respuestas duraderas alcanza supervivencias superiores a 10 años, apoyando el concepto de cura funcional.
Conclusión: la integración de datos multiómicos y la actualización de las escalas pronósticas permitirán avanzar hacia una medicina de precisión, incrementando las remisiones prolongadas y reduciendo la toxicidad del tratamiento continuo.
Visitas del artículo 0 | Visitas PDF 0
Descargas
- Ludwig H, Novis Durie S, Meckl A, Hinke A, Durie B. Multiple myeloma incidence and mortality around the globe: interrelations between health access and quality, economic resources, and patient empowerment. Oncologist [Internet]. 2020;25(9):e1406–e1413. Disponible en: https://doi.org/10.1634/theoncologist.2020-0141
- Siegel RL, Kratzer TB, Giaquinto AN, Sung H, Jemal A. Cancer statistics, 2025. CA Cancer J Clin [Internet]. 2025;75(1):10–45. Disponible en: https://doi.org/10.3322/caac.21871
- International Agency for Research on Cancer. GLOBOCAN 2022: Colombia fact sheet. Global Cancer Observatory [Internet]. 2022. Disponible en: https://gco.iarc.who.int.
- Cuenta de Alto Costo. Informe especial: neoplasias hematológicas en el marco del aseguramiento en Colombia. [Internet]. 2025. Disponible en: https://cuentadealtocosto.org
- Palumbo A, Anderson K. Multiple myeloma. N Engl J Med [Internet]. 2011;364(11):1046–1060. Disponible en: https://doi.org/10.1056/NEJMra1011442
- Surveillance, Epidemiology, and End Results Program. Cancer stat facts: myeloma. [Internet]. Disponible en: https://seer.cancer.gov/statfacts/html/mulmy.html
- Avet-Loiseau H, Attal M, Campion L, et al. Long-term analysis of the IFM 99 trials for myeloma: cytogenetic abnormalities play a major role in defining long-term survival. J Clin Oncol [Internet]. 2012;30(16):1949–1952. Disponible en: https://doi.org/10.1200/JCO.2011.36.5726
- Pasvolsky O, Wang Z, Milton DR, et al. Multiple myeloma patients with a long remission after autologous hematopoietic stem cell transplantation. Blood Cancer J [Internet]. 2024;14(1):82. Disponible en: https://doi.org/10.1038/s41408-024-01062-2
- Kasomva K, Yadav K, Janz S, Dhakal B, Rao S. Molecular and immunological determinants of long-term survival in multiple myeloma. Blood Adv [Internet]. 2025. Disponible en: https://doi.org/10.1182/bloodadvances.2025016829.
- Gong L, Qiu L, Hao M. Novel insights into the initiation, evolution, and progression of multiple myeloma by multi-omics investigation. Cancers (Basel) [Internet]. 2024;16(3):498. Disponible en: https://doi.org/10.3390/cancers16030498
- Heider M, Nickel K, Högner M, Bassermann F. Multiple myeloma: molecular pathogenesis and disease evolution. Oncol Res Treat [Internet]. 2021;44(12):672–681. Disponible en: https://doi.org/10.1159/000520312
- Xu A, Guo T, Zhang S, et al. Prevalence of monoclonal gammopathy of undetermined significance in Shenzhen, China. Hematology [Internet]. 2024;29(1):2352686. Disponible en: https://doi.org/10.1080/16078454.2024.2352686
- Landgren O, Kyle RA, Pfeiffer RM, et al. Monoclonal gammopathy of undetermined significance consistently precedes multiple myeloma: a prospective study. Blood [Internet]. 2009;113(22):5412–5417. Disponible en: https://doi.org/10.1182/blood-2008-12-194241
- van Nieuwenhuijzen N, Spaan I, Raymakers R, Peperzak V. From MGUS to multiple myeloma, a paradigm for clonal evolution of premalignant cells. Cancer Res [Internet]. 2018;78(10):2449–2456. Disponible en: https://doi.org/10.1158/0008-5472.can-17-3115
- Fonseca R, Debes-Marun CS, Picken EB, et al. The recurrent IgH translocations are highly associated with nonhyperdiploid variant multiple myeloma. Blood [Internet]. 2003;102(7):2562–2567. Disponible en: https://doi.org/10.1182/blood-2003-02-0493
- Prideaux SM, Conway O’Brien E, Chevassut TJ. The genetic architecture of multiple myeloma. Adv Hematol [Internet]. 2014;2014:864058. Disponible en: https://doi.org/10.1155/2014/864058
- Smadja NV, Fruchart C, Isnard F, et al. Chromosomal analysis in multiple myeloma: cytogenetic evidence of two different diseases. Leukemia [Internet]. 1998;12(6):960–969. Disponible en: https://doi.org/10.1038/sj.leu.2401041
- Testa U, Pelosi E, Castelli G, Leone G. Recent advances in the definition of the molecular alterations occurring in multiple myeloma. Mediterr J Hematol Infect Dis [Internet]. 2024;16(1):e2024062. Disponible en: https://doi.org/10.4084/MJHID.2024.062
- Ntanasis-Stathopoulos I, Terpos E, Malandrakis P, et al. Prognostic impact of t(11;14) in newly diagnosed patients with multiple myeloma in the era of modern treatments. Blood [Internet]. 2024;144:6968. Disponible en: https://doi.org/10.1182/blood-2024-202627
- Hebraud B, Magrangeas F, Cleynen A, et al. Role of additional chromosomal changes in the prognostic value of t(4;14) and del(17p) in multiple myeloma. Blood [Internet]. 2015;125(13):2095–2100. Disponible en: https://doi.org/10.1182/blood-2014-07-587964
- De Novellis D, Scala P, Giudice V, Selleri C. High-risk genetic multiple myeloma: from molecular classification to innovative treatment with monoclonal antibodies and T-cell redirecting therapies. Cells [Internet]. 2025;14(11). Disponible en: https://doi.org/10.3390/cells14110776
- Chapman MA, Lawrence MS, Keats JJ, et al. Initial genome sequencing and analysis of multiple myeloma. Nature [Internet]. 2011;471(7339):467–472. Disponible en: https://doi.org/10.1038/nature09837
- Shah V, Sherborne AL, Walker BA, et al. Prediction of outcome in newly diagnosed myeloma: a meta-analysis of the molecular profiles of 1905 trial patients. Leukemia [Internet]. 2018;32(1):102–110. Disponible en: https://doi.org/10.1038/leu.2017.179
- Walker BA, Mavrommatis K, Wardell CP, et al. A high-risk, double-hit, group of newly diagnosed myeloma identified by genomic analysis. Leukemia [Internet]. 2019;33(1):159–170. Disponible en: https://doi.org/10.1038/s41375-018-0196-8
- D’Agostino M, Cairns DA, Lahuerta JJ, et al. Second revision of the International Staging System (R2-ISS) for overall survival in multiple myeloma: A European Myeloma Network (EMN) report within the HARMONY Project. J Clin Oncol [Internet]. 2022;40(29):3406–3418. Disponible en: https://doi.org/10.1200/jco.21.02614
- Avet-Loiseau H, Davies FE, Samur MK, et al. International Myeloma Society/International Myeloma Working Group Consensus recommendations on the definition of high-risk multiple myeloma. J Clin Oncol [Internet]. 2025;43(24):2739–2751. Disponible en: https://doi.org/10.1200/jco-24-01893
- Terebelo HR, Omel J, Wagner LI, et al. Characteristics and Treatment Patterns of Long-surviving Patients With Multiple Myeloma: Over 13 Years of Follow-up in the ConnectⓇ MM Registry. Clin Lymphoma Myeloma Leuk [Internet]. 2025;25(1):58–66. Disponible en: https://doi.org/10.1016/j.clml.2024.11.001
- Vu T, Gonsalves W, Kumar S, et al. Characteristics of exceptional responders to lenalidomide-based therapy in multiple myeloma. Blood Cancer J [Internet]. 2015;5(10):e363. Disponible en: https://doi.org/10.1038/bcj.2015.91
- Paner A, Patel P, Dhakal B. The evolving role of translocation t(11;14) in multiple myeloma. Blood Rev [Internet]. 2020;41:100643. Disponible en: https://doi.org/10.1016/j.blre.2019.100643
- Atamaniuk J, Gleiss A, Porpaczy E, et al. Overexpression of G protein-coupled receptor 5D in the bone marrow is associated with poor prognosis in multiple myeloma. Eur J Clin Invest [Internet]. 2012;42(9):953–960. Disponible en: https://doi.org/10.1111/j.1365-2362.2012.02679.x
- Rodriguez-Otero P, van de Donk NWCJ, Pillarisetti K, et al. Correction: GPRC5D as a novel target for the treatment of multiple myeloma. Blood Cancer J [Internet]. 2024;14(1):40. Disponible en: https://doi.org/10.1038/s41408-024-01018-6
- Rodriguez-Otero P, van de Donk NWCJ, Pillarisetti K, et al. GPRC5D as a novel target for the treatment of multiple myeloma. Blood Cancer J [Internet]. 2024;14(1):24. Disponible en: https://doi.org/10.1038/s41408-024-01018-6
- Frerichs KA, Broekmans MEC, Marin Soto JA, et al. Preclinical activity of JNJ-7957, a novel BCMA×CD3 bispecific antibody. Clin Cancer Res [Internet]. 2020;26(9):2203–2215. Disponible en: https://doi.org/10.1158/1078-0432.ccr-19-2299
- Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol [Internet]. 2020;21(2):207–221. Disponible en: https://doi.org/10.1016/S1470-2045(19)30788-0
- Munshi NC, Anderson LD, Shah N, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med [Internet]. 2021;384(8):705–716. Disponible en: https://doi.org/10.1056/NEJMoa2024850
- Berdeja JG, Madduri D, Usmani SZ, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet [Internet]. 2021;398(10297):314–324. Disponible en: https://doi.org/10.1016/S0140-6736(21)00933-8
- Waldschmidt JM, Rasche L, Kortüm KM, Einsele H. Comprehensive review of bispecific antibody constructs in multiple myeloma. Clin Lymphoma Myeloma Leuk [Internet]. 2025;25(5):309–315. Disponible en: https://doi.org/10.1016/j.clml.2024.11.012
- Kumar SK, Rajkumar V, Kyle RA, et al. Multiple myeloma. Nat Rev Dis Primers [Internet]. 2017;3:17046. Disponible en: https://doi.org/10.1038/nrdp.2017.46
- Chesi M, Bergsagel PL. Molecular pathogenesis of multiple myeloma: basic and clinical updates. Int J Hematol [Internet]. 2013;97(3):313–323. Disponible en: https://doi.org/10.1007/s12185-013-1291-2
- Moreau P, Cavo M, Sonneveld P, et al. Combination of International Scoring System 3, High Lactate Dehydrogenase, and t(4;14) and/or del(17p) Identifies Patients With Multiple Myeloma (MM) Treated With Front-Line Autologous Stem-Cell Transplantation at High Risk of Early MM Progression–Related Death. J Clin Oncol [Internet]. 2014;32(20):2173–2180. Disponible en: https://doi.org/10.1200/jco.2013.53.0329
- Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised International Staging System for multiple myeloma: A Report From International Myeloma Working Group. J Clin Oncol [Internet]. 2015;33(26):2863–2869. Disponible en: https://doi.org/10.1200/JCO.2015.61.2267
- Zanwar S, Rajkumar SV. Current risk stratification and staging of multiple myeloma and related plasma cell disorders. Leukemia [Internet]. 2025. Disponible en: https://doi.org/10.1038/s41375-025-02654-y

















